Newborn sleep patterns: A survival guide

As every parent knows, the world of newborn sleep is exotic and strange. Babies rack up lots of sleep overall, averaging 16-18 hours a day during the first two weeks. Yet they awaken frequently, and rarely sleep more than 4 hours at a stretch, even at night. Their internal clocks aren’t yet synchronized with the external, 24-hour day.

It’s a recipe for exhaustion, but understanding the science of sleep can help you cope, and avoid mistakes that can delay your child’s development of more mature sleep rhythms. In this article, you’ll learn about
- fundamental differences between newborn sleep and adult sleep;
- circadian rhythms, and how you can help your baby get in sync with the natural day;
- sleep cycles in the newborn, and how to work around them;
- tips for preventing newborns from waking up; and
- advice for improving your own sleep.
Throughout, I focus on babies under four weeks of age. For information about older infants, see my article on baby sleep patterns. If you are looking for information about newborn sleep safety, see these science-based tips for reducing the risk of SIDS.
Overview: What can parents expect?
Newborn sleep may look totally disorganized, and no wonder. The sleep patterns of young babies differ from adult sleep in several important ways.
For example, newborns sleep at odd times, and never for very long. Instead of sleeping primarily at night (as most older people do), newborns sleep at seemingly random times throughout the 24-hour day. Their sleep bouts can be very brief (lasting only a few minutes), and seldom last more than 3-4 hours.
In addition, once awakened, newborns often have difficulty falling back to sleep on their own. As I explain elsewhere, it’s normal for everyone (adults included) to experience many arousals during the night, and, when things are going well, these night wakings are not disruptive. We quickly resume sleeping. Newborns experience many night wakings as well, but they tend to lack the ability to “self-soothe” — or settle themselves back to sleep without crying and signaling caregivers.
Moreover, newborn sleep looks quite different from the outside. Compared with adult sleep, newborn sleep can be very restless. That’s because babies spend a large portion of their sleep-time in “active sleep,” a light sleep stage characterized by
- fluttering eyelids;
- rapid, irregular breathing;
- frequent twitches and body movements; and even
- vocalizations (such as grunts and brief cries).
The movements and noise can sometimes fool parents into thinking their babies are awakening or signalling for attention — a complication that can lead us to intervene when it isn’t necessary. (Read more about it in my article, “Baby sleep stages: What is active sleep and quiet sleep?”)
What else should you be prepared for? A great deal of individual variation!
Newborns sleep a lot, but they aren’t all the same. For instance, during the first two months postpartum, the average baby sleeps about 14-15 hours every 24 hours. Yet some parents have reported a little as 9-10 hours, and others – especially in the first days postpartum – have noted that their babies sleep 16-18 hours or more (Sadeh et al 2009; Galland et al 2012; Pecora et al 2022).
Put it all together, and sounds pretty chaotic, right? But if you learn about circadian rhythms and sleep cycles, you can start to make sense of your baby’s sleep habits, and lay the groundwork for easier nights.
Part One. Developing circadian rhythms: Why newborns seem to sleep—and wake—at erratic times
For adults, the timing of sleep is governed by circadian rhythms — physiological changes that follow a 24-hour cycle. In effect, we have an internal clock…a tiny pacemaker in our brains known as the “suprachiasmatic nucleus,” or SCN. And when everything is functioning properly, the SCN helps make us feel alert during the daytime and sleepy at night.
How does it work? How does the SCN know what time it is? We aren’t born with this information. The SCN isn’t “hard-wired” with pre-programmed waking and sleeping times. Instead, the system depends on environmental cues, or “zeitgebers,” to tune the internal clock. And the most powerful zeitgeber for the SCN is light. Especially the light that enters our eyes.
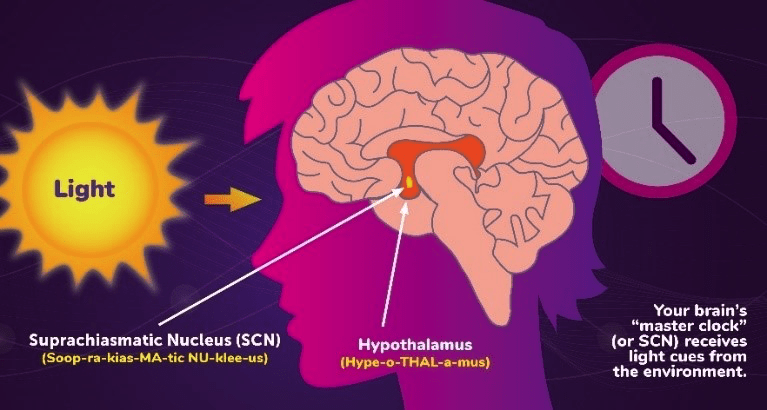
For instance, when you expose yourself to bright light during the day, you are helping the SCN calibrate itself. Even if you are feeling tired and sleep-deprived, the SCN will forward the message to the rest of the body: It’s time to be awake. Conversely, when darkness falls, the SCN interprets this as a signal for your brain to produce melatonin — the hormone that triggers relaxation, paving the way for sleep.
It’s a system that allows us to adapt to changes, including the sudden shifts we experience when we fly to a new time zone. Feeling jet lagged? As long as you expose yourself to the right zeitgebers, you can get your circadian rhythms in sync with your new time zone. It just takes a little time – about one day for every time zone crossed, give or take (Eastman and Burgess 2009).
Sounds hopeful, right? And you might be forgiven for thinking it should be easy to get your newborn on track. In the last 10 weeks before birth, babies seem to share the circadian rhythms of their mothers. Hormones like melatonin can pass from mother to fetus through the placenta (Torres-Farfan et al 2006; Logan and McClung 2019), and fetal heart rates synchronize with the mother’s activity levels – speeding up during the day, and slowing down at night (Mirmiran et al 2003).
But at the moment of birth, this changes. Babies are suddenly cut off from their mothers’ intimate physiological signals. Now they must begin to generate their own, internal, circadian rhythms, and this is challenging for several reasons.
1. Newborns need to feed every 3-4 hours, which awakens parents and sets the stage for disrupting the rhythms of the whole family.
If caregivers handle night wakings by turning on the lights or making noise, they send the wrong message to the newborn brain — potentially delaying their babies’ circadian development.
2. Modern lifestyles may lead parents (however unwittingly) to make choices that deprive our babies of cues about daytime.
Our ancestors lived outdoors, and they carried their infants with them as they foraged and worked. So babies were exposed to lots of daylight, and plenty of bustling, daytime social activity – important zeitgebers to get the internal clock on track (Wong et al 2022). By contrast, in contemporary societies, newborns spend most of their lives indoors, and infants are less likely to “tag along”, or be included in, the routine activities of other family members (e.g., van Schaik et al 2020).
3. Some babies may be getting the wrong chemical cues.
As I explain in another article, breast milk contains a number of circadian, chemical cues that vary over the 24-hour day. When infants consume formula instead of breast milk, they miss out on these cues. And if we bottle-feed our babies with breast milk that was pumped at the “wrong” time of day, we might be undermining the development of circadian rhythms – giving babies “sleepy” milk in the morning, or “wake-up” milk in the evening.
4. The internal clock of the newborn — the SCN — is still developing.
It has only a small fraction of the neurons found in an adult’s SCN, so we might expect newborns to have more difficulty adjusting – even in the presence of appropriate zeitgebers.
When do babies develop mature circadian rhythms?

Research suggests that many babies aren’t producing surges of nighttime melatonin until around 9-15 weeks postpartum (Kenneway et al 1996; Joseph et al 2015). This timing meshes with observations about how long it takes babies to “settle” at night, or sleep for at least 5 hours uninterrupted. According to several studies, babies take approximately 3-5 months to achieve that milestone (Teng et al 2012; Sadeh et al 2009; Jenni et al 2006; Pinilla and Birch 1993).
But melatonin release is just one biological process affecting your baby’s circadian rhythms, and some circadian changes may begin earlier than 9 weeks. In fact, investigators have found that even brand-new babies can possess a bias for sleeping a bit more at night than during the day (Freudigman and Thoman 1998; Korte 2004; Matsuoka et al 1991).
What’s the takeaway? More science – more research – is needed for us to fully understand how babies develop circadian rhythms. But given what we know so far, it makes sense to provide your newborn with the kind of environment that is most supportive of developing mature circadian rhythms. Here are some tactics to consider.
Tips: How to support the development of circadian rhythms in babies
1. Expose your newborn to natural lighting patterns.
In one study, newborns slept longer at night if their parents observed a regular policy of turning out the lights by 9pm (Iwata et al 2017). In another study, young babies tended to sleep longer at night if they had been exposed to lots of early afternoon light (Harrison 2004). And time spent outdoors might make an important difference. Babies who go outside experience much higher daytime light levels than those kept indoors all day, and may develop stronger circadian rhythms as a result (Tsai et al 2012).
2. Try to avoid darkening the room during daytime naps.
Although I haven’t seen any controlled studies testing the effects of napping in the darkness, there are good reasons to question the practice. For instance, it’s pretty clear that light can penetrate the eyelids and affect circadian rhythms (Figueiro 2015), so it’s possible that napping in a darkened room could confuse the internal clock – sending the message that it’s actually nighttime.
3. Make your baby a part of your daytime routine.
Research suggests that daily social interactions can have their own, distinct effects on circadian rhythms (Mistlberger and Skene 2004), and, when parents include their newborns in their daily activities, babies may adapt more rapidly to the 24-hour day (Custodio et al 2007; Lorh et al 1999). One study took continuous measurements of mother-infant activity patterns for four months after birth. Newborns who were active at the same time of day as their mothers were quicker to develop mature circadian rhythms (Wulff and Siegmund 2002).
4. Reduce social stimulation at night.
Too much social stimulation at night can send the message that it’s time to be awake and engaged, so when your baby wakes for night time feedings, keep activity to a minimum. Make as little noise as possible, and avoid moving your baby around. Your goal is to keep your baby in a drowsy state, and make it easy for him or her to fall back to sleep.
5. Consider the benefits of breastfeeding, and – if you pump your milk – pay attention to the timing of milk production.
During morning sessions of bottle-feeding, give your baby milk that was originally expressed in the morning. At night, give your baby milk that was originally produced at night.
Part Two. Understanding sleep stages and sleep cycles

Chances are, you’ve already heard something about adult sleep cycles, and it’s helpful to review this in order to make sense of newborn sleep.
When adults first fall drowse off, we pass through a couple of light sleep stages (NREM1 and NREM2), and then plunge into a bout of deep sleep (NREM3), during which we experience slow, rhythmic, brain activity. This is the type of sleep that the brain prioritizes when we are sleep deprived. Next, we make a brief trip back into light sleep before entering REM, or “rapid eye movement” sleep – a stage associated with high levels of brain activity, many dreams, and sleep paralysis. We’re pretty unresponsive during REM, and we don’t move around. Finally, when this REM stage is over, we either awaken, or return to light sleep and begin the cycle again. The whole sequence can be summarized this way:
- NREM1
- NREM2
- NREM3
- NREM2
- REM
For most adults, a single sleep cycle lasts between 90 – 110 minutes, and, in a typical night, we experience between 4 and 6 such cycles in a row. As the night wears on, we spend progressively more time in NREM2 and REM, and less time in NREM3. In general, most adults spend approximately 20-25% of their total sleep time in REM, and 15-25% in deep sleep (Colten and Altevogt 2006).
Do we sleep continuously throughout the night? Not exactly. It’s normal to experience many partial awakenings, or “arousals” — most commonly during stages of light sleep and during the transition between sleep stages. For example, on average, adults in their thirties and forties experience approximately 17 arousals per hour (Bonnet and Arand 2007). But most of these episodes are very brief — lasting only a few seconds or less — and we don’t typically remember them the next day.
Okay. So what about newborns?
Newborn sleep is also marked by sleep stages and sleep cycles, but there are crucial differences.

We can get a feeling for this by considering some of the numbers. Newborn sleep cycles are shorter — around 50-55 minutes — and the newborn version of REM (called “active sleep”) takes up a much bigger portion of sleep-time. It’s not unusual for newborns to spend more than half their total sleep time in REM (Grigg-Damberger 2016). Indeed, several studies suggest that, over the course of a 24 hour day, some newborns spent may spend as much as 75% of their sleep time in this active sleep stage (e.g., Poblano et al 2007; Sadeh et al 1996).
And there’s more. We’ve noted how adults in REM means are pretty unresponsive and immobile, but that’s not how it works in young babies. As I’ve mentioned in the introduction, newborns tend to twitch, move, and even cry out during active sleep. They can make facial expressions, too (Grigg-Damberger 2016; Barbeau and Weiss 2017).
All that physical activity can jolt babies awake, which is probably why newborns experience such a high rate of arousals during REM or active sleep. In one EEG study of young infants, babies in REM experienced cortical arousals at an average rate of 32 per hour – more than one arousal every two minutes (McNamara et al 2002)!
What about other sleep stages? For newborns, the main alternative is a type of non-REM called “quiet sleep”, which – as you might expect – looks more restful. Except for the occasional twitch, babies stop thrashing around. There are no eye movements. Breathing and heart rates become regular, and the rate of cortical arousals drops by nearly 50% (McNamara et al 2002).
In addition, during the transitions between active sleep and quiet sleep, babies often experience brief intervals of “indeterminate sleep” (or “IS”), sleep that researchers find hard to categorize, because it combines features of REM (like movements and vocalizations) with features of non-REM (like regular breathing). How does this all come together?
How newborn sleep stages unfold
When researchers have monitored newborns with sleep polysomnography — a technique that includes measuring electrical brain activity with an EEG, they have observed a regular sequence that babies tend to follow after dozing off (Dereymaeker et al 2017). Newborn sleep doesn’t always follow this pattern. But this is what’s typical:
- Active sleep. The baby dozes off and begins a bout of newborn REM.
- Indeterminate sleep. The baby may continue to move around or vocalize during sleep.
- Quiet sleep. The baby finally sleeps in a more quiet, immobile, peaceful-looking mode.
- Indeterminate sleep. Movements and vocalizations become more common again.
- Active sleep. The baby enters a second bout of active REM.
- Brief (60-90 second) episode of waking. Typically, a baby will awaken from active sleep for a minute or more.
- Indeterminate sleep. This is usually the last stage of the sleep cycle – a brief return to indeterminate sleep.
It might look complicated, but we can sum it up in a simple way. When newborns are sleeping, they are likely to twitch, move, and vocalize, and they can awaken rather easily. The exception is during the middle of a sleep cycle, when — for around 20 minutes — babies enter quiet sleep.
Why are newborns like this?
It’s a good question. Why is newborn REM so unstable and rambunctious? And why do babies devote so much of their sleep-time to REM?
Fascinating research suggests that REM serves a special function for young infants. As it turns out, it isn’t only human babies that spend so much time in REM. This is a common pattern in many mammalian species (Frank 2020). And biologists think that young infants might need all that muscle-twitching to help develop crucial motor circuits in the brain. In effect, newborns may be testing the “wiring” — discovering how different parts of the brain are connected with body movements and sensations (Roffwarg et al 1966; Frank 2020; Seigel 2005).
In addition, studies suggest that REM is linked with larger brain volume and memory performance. When infants experience deficiencies in REM, they are more likely to suffer from developmental disabilities and behavior problems (Chen et al 2022). And there’s reason to think that sleeping light may have an immediate, protective effect for newborns — especially during episodes when babies experience lower oxygen levels. When researchers have challenged sleeping babies with a sudden reduction in oxygen, they’ve found that babies respond differently, depending on whether they are in active sleep or quiet sleep. Babies are slower to awaken from quiet sleep (Parslow et al 2003; Damberger et al 2007).
This, then, may explain why newborns don’t oblige exhausted parents by lapsing into long periods of deep sleep. Babies need to keep moving and twitching for optimal brain development. And spending long stretches of time in quiet sleep could be risky. So instead, the typical 50-55 minute newborn sleep cycle includes only about 20 minutes of quiet sleep.
What can parents do to cope with newborn sleep cycles?
There’s no doubt about it. Taking care of a young baby will disrupt your sleep patterns — especially during those first weeks postpartum. But we can use our knowledge of sleep cycles — in both adults and babies — to minimize the disruption, and avoid needless mistakes. So let’s review two sets of tips — one for taking care of your baby, and the other for taking care of yourself.

Tips: How to keep your light sleeper from waking up all the way
1. “Tank up” the baby before you go to sleep.
Whether you breastfeed or bottle-fed, try to give the baby an especially large meal before your own bedtime. This will encourage your baby to sleep longer. To learn more about this approach, see this Parenting Science guide to “Dream feeding.”
2. Don’t rush in the moment you think your baby has awakened.
As noted above, babies experience frequent arousals, but that doesn’t mean they are doomed to wake up “all the way” every few minutes. Babies often jerk, sigh, or vocalize during partial arousals. If you avoid stimulating them during these moments, they may go back to sleep on their own.
3. Did you soothe a crying baby to sleep in your arms? Try this before attempting to transfer your baby to bed.
Babies are often awakened by the act of detaching from our bodies, but that doesn’t mean we have to give up on the idea of laying them down. In a recent study, sleeping babies were more likely to remain asleep if parents waited at least 8.5 minutes before attempting to transfer them to a crib or cot (Ohmura et al 2022). We need more research to corroborate this, but the results are consistent with the idea that babies begin dozing in a bout of light sleep. If we can wait until our babies are sleeping more deeply, we may be able to avoid awakening our babies when we put them to bed. For more information, see my article, “How to soothe a crying baby to sleep”.
4. Learn about bedtime routines and other tactics for promoting infant sleep.
My article on infant sleep aids includes tips for improving newborn sleep, and avoiding practices that are either unhelpful or potentially hazardous.
What about you? Tips for improving your own sleep
Newborn sleep patterns take their toll on parents. In a study tracking the sleep patterns of mothers from pregnancy through the postpartum period, maternal sleep worsened after childbirth and continued to deteriorate until about 12 weeks postpartum (Kang et al 2002)–the time when newborn sleep patterns begin to show marked circadian rhythms (Nishihara et al 2000).
Twelve weeks isn’t forever, but it can seem like it when you are severely sleep restricted. As you struggle to cope with newborn sleep patterns, don’t forget to look after yourself. Here are some tips to help you cope.

1. Do what you can to protect that first sleep cycle of the night.
Parents naturally wonder. Is it better to sleep well at the beginning of the night, or at the end? And sleep science has an answer: When you’re sleep-deprived, you’re likely to reap the most benefits — rack up the most intense, restorative, slow-wave sleep — during that first sleep cycle of the night. That’s because the brain gives NREM3 special emphasis during the first sleep cycle. Thereafter, it tends to allocate ever-less time to this sleep stage. In fact, by the last sleep cycle, you’ll likely spend most of your time in light sleep and REM, with very little NREM3. So if you can protect only one part of the night from interruptions and wakings, focus on the first 2-3 hours.
2. Appreciate the power of a 30-minute nap
When you’re running up an enormous sleep debt, you might think a 30-minute nap will make little difference to your health. But research confirms that all naps are not the same. When you’re sleep deprived, the brain compensates by rendering naps more restorative than usual.
In one study, volunteers permitted to sleep only 2 hours at night showed the typical abnormalities in their stress hormone and immune factor chemistry. But after just two 30-minute naps, those irregularities were entirely normalized (Faraut et al 2015b). In another study, volunteers coping with a 2-hour nightly regimen experienced heightened pain sensitivity — a common symptom of sleep deprivation. But once again, the effect was reversed after just two 30-minute naps (Faraut et al 2015a).
3. Don’t assume that it’s pointless to lie down if you don’t fall asleep. You might pass into a state of drowsy, semi-conscious sleep — and reap some benefits.
Too wired to “sleep when the baby sleeps”? If so, keep in mind that quiet resting is better than nothing. In fact, if you are lying down with your eyes closed, you might be asleep without realizing it.
In numerous lab studies, subjects who were awakened from the first stage of sleep often denied that they were asleep at all (Dement and Vaughan 1999). A nap that consists only of NREM1 might not help you improve your reaction times, but it will probably make you feel less tired. And if you manage to slip into NREM2 — even for just 3 minutes — your nap may have recuperative effects (Hayashi et al 2005).
4. Don’t play the blame game.
Brooding about the situation will make it harder for you to fall asleep when you are given the opportunity. And it’s wrong-headed, too: You might be doing everything you can to get more sleep, and still be stuck with a baby who sleeps less than average. Research suggests that the amount of sleep we get at night is strongly influenced by genetics (Touchette et al 2013), and, as mentioned above, there is a lot of individual variation among newborns.
5. Don’t assume that breastfeeding your newborn will make you more sleepless than formula feeding.
Researchers have monitored the sleep of new parents by asking them to self-report. They’ve also asked parents to wear wrist actigraphs — providing objective data about how long these tired folks actually sleep. And in comparisons of breastfeeding- and formula-feeding parents, parents who breastfeed tend to experience less nighttime sleep loss (Srimoragot et al 2022).
For example, in one study researchers measured maternal sleep in the last month before childbirth, and once again when babies were 4 weeks old. Sleep loss is already pretty bad during pregnancy, so the question was: How much worse did things get after the baby arrived? And the answer depended on feeding. Mothers who breastfed exclusively were sleeping an average of 21 minutes less at night than they had during late pregnancy. By contrast, mothers who formula-fed were coping with an average nighttime sleep decrease of 62 minutes (Doan et al 2014).
6. If your baby is asleep, don’t worry about changing diapers.
If your baby can’t sleep because she needs a diaper change, she’ll let you know. And a little urine is unlikely to awaken her anyway. In a recent experiment, researchers injected water into the diapers of sleeping infants to see if this would wake them up (Zotter et al 2007). It didn’t.
7. Get sunlight and avoid artificial lighting at night.
As noted above, natural lighting helps influence newborn sleep patterns. But it also helps you keep your own circadian rhythms from drifting, which is important if you are going avoid insomnia and be a source of daytime cues for your newborn. So expose yourself to bright light during the day, and dim the electric lights before bedtime.
8. Let a friend or family member watch your baby while you take a nap, even if this means your breastfed baby will take some meals from a bottle.
Lactation experts often discourage breastfeeding mothers from bottle feeding babies for the first 3-4 weeks. The worry is that supplemental feeds will lead to a decreased milk supply and endanger successful breastfeeding in the long-term.
But you need to balance this against the negative effects of severe sleep restriction. Lack of sleep puts parents at increased risk of illness and postpartum depression, which is bad for parents and babies. If you are at the end of your rope, get help.
9. Trust your instincts, and get help when you feel stressed
If something feels wrong with you or the baby, talk to your physician. And remember that your own mental health is crucial. Coping with sleep deprivation is very stressful, especially if your infant seems to be especially fussy or prone to crying. Watch for signs of postpartum stress and postpartum depression, and reach out to others for support.
10. Remember that things will get better
Newborns have special sleep patterns and special needs. But things will start to get better around 12 weeks postpartum.
More reading relevant to newborn sleep
For more information about babies and sleep, see these fully referenced Parenting Science articles:
References: What scientific studies say about newborn sleep
Anders TF. 1979. Night-waking in infants during the first year of life. Pediatrics 63: 860-864.
Bennett C, Underdown A, and Barlow J. 2013. Massage for promoting mental and physical health in typically developing infants under the age of six months. Cochrane Database Syst Rev. 2013 (4):CD005038. doi: 10.1002/14651858.CD005038.pub3.
Booker LA, Spong J, Deacon-Crouch M, Skinner TC. 2022.Preliminary exploration into the impact of mistimed expressed breast milk feeding on infant sleep outcomes, compared to other feeding patterns. Breastfeed Med. 17(10):853-858.
Caba-Flores MD, Ramos-Ligonio A, Camacho-Morales A, Martínez-Valenzuela C, Viveros-Contreras R, Caba M. 2022. Breast Milk and the Importance of Chrononutrition. Front Nutr. 9:867507.
Cheruku SR, Montgomery-Downs HE, Farkas SL, Thoman EB, and Lammi-Keefe CJ. 2002. Higher maternal plasma docosahexaenoic acid during pregnancy is associated with more mature neonatal sleep-state patterning. Am J Clin Nutr 76:608-13.
Colten HR and Altevogt BM (eds). 2006. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Institute of Medicine (US) Committee on Sleep Medicine and Research. Washington (DC): National Academies Press (US).
Coons S and Guilleminault C. 1984. Development of consolidated sleep and wakeful periods in relation to the day/night cycle in infancy. Dev. Med. Child. Neurol. 26:169–176.
Cubero J, Valero V, Sánchez J, Rivero M, Parvez H, Rodríguez AB, Barriga C. 2005. The circadian rhythm of tryptophan in breast milk affects the rhythms of 6-sulfatoxymelatonin and sleep in newborn. Neuro Endocrinol Lett. 26(6):657-61.
Cubero J, Narciso D, Terrón P, Rial R, Esteban S, Rivero M, Parvez H, Rodríguez AB, Barriga C. 2007. Chrononutrition applied to formula milks to consolidate infants’ sleep/wake cycle. Neuro Endocrinol Lett. 28(4):360-6.
Custodio RJ, Junior CE, Milani SL, Simões AL, de Castro M, Moreira AC. 2007. The emergence of the cortisol circadian rhythm in monozygotic and dizygotic twin infants: the twin-pair synchrony. Clin Endocrinol (Oxf). 66(2):192-7.
Dement W and Vaughan C. 1999. The promise of sleep. New York: Random House.
Doan T, Gay CL, Kennedy HP, Newman J, Lee KA. 2014. Nighttime breastfeeding behavior is associated with more nocturnal sleep among first-time mothers at one month postpartum. J Clin Sleep Med. 10(3):313-9.
Doan T, Gardiner A, Gay CL, Lee KA. 2007 Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs. 21(3):200-6.
Eastman CI and Burgess HJ. 2009. How To Travel the World Without Jet lag. Sleep Med Clin. 4(2):241-255.
Faglioli I, Barconcini P, Ricour C, and Salzarulo P. 1998. Decrease of slow-wave sleep in children with prolonged absence of essential lipids intake. Sleep 12: 495-499.
Faraut B, Léger D, Medkour T, Dubois A, Bayon V, Chennaoui M, Perrot S. 2015a. Napping reverses increased pain sensitivity due to sleep restriction. PLoS One. 10(2):e0117425.
Faraut B, Nakib S, Drogou C, Elbaz M, Sauvet F, De Bandt JP, Léger D. 2015b. Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction. J Clin Endocrinol Metab. 100(3):E416-26.
Ferber SG, Laudon M, Kuint J, Weller A, Zisapel N. 2002. Massage therapy by mothers enhances the adjustment of circadian rhythms to the nocturnal period in full-term infants. J Dev Behav Pediatr. 23(6):410-5.
Field T, Gonzalez G, Diego M, Mindell J. 2016. Mothers massaging their newborns with lotion versus no lotion enhances mothers’ and newborns’ sleep. Infant Behav Dev. 45(Pt A):31-37.
Freudigman KA and Thoman EB. 1998. Infants’ earliest sleep/wake organization differs as a function of delivery mode. Dev Psychobiol. 32(4):293-303.
Galland BC, Taylor BJ, Elder DE, Herbison P. 2012. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 16(3):213-22.
Grigg-Damberger MM. 2016. The Visual Scoring of Sleep in Infants 0 to 2 Months of Age. J Clin Sleep Med. 12(3):429-45.
Iglowstein I, Jenni OG, Molinari L, Largo RH. 2003. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 111(2): 302-307.
Harrison Y. 2004. The relationship between daytime exposure to light and night-time sleep in 6-12-week-old infants. J Sleep Res. 13(4):345-52.
Hayashi M, Motoyoshi N, Hori T. 2005. Recuperative power of a short daytime nap with or without stage 2 sleep. Sleep. 28(7):829-36.
Heraghty JL, Hilliard TN, Henderson AJ, and Fleming PJ. 2008. The physiology of sleep in infants. Arch Dis Child. 2008 Nov;93(11):982-5.
Horne RSC, Parslow PM, Ferens D, Watts AM, and Adamson TM. 2004. Comparison of evoked arousability in breast and formula fed infants. Arch Dis Child 89: 22-25.
Hugelin A. 1982. Mechanisms of respiratory control during sleep and wakefulness: implications in newborn sleep apnoea. Electroencephalogr Clin Neurophysiol Suppl. 36:625-30.
Iwata S, Fujita F, Kinoshita M, Unno M, Horinouchi T, Morokuma S, Iwata O. 2017. Dependence of nighttime sleep duration in one-month-old infants on alterations in natural and artificial photoperiod. Sci Rep. 7:44749.
Jenni OG, DeBoer T, and Acherman P. 2006. Development of the 24h rest-activity pattern in human infants. Infant behavior and development 29: 143-152.
Joseph D, Chong NW, Shanks ME, Rosato E, Taub NA, Petersen SA, Symonds ME, Whitehouse WP, Wailoo M. 2015. Getting rhythm: how do babies do it? Arch Dis Child Fetal Neonatal Ed. 100(1):F50-4.
Kang MJ, Matsumoto K, Shinkoda H, Mishima M, Yeo YJ. 2002. Longitudinal study for sleep-wake behaviours of mothers from pre-partum to post-partum using actigraph and sleep logs. Psychiatry Clin Neurosci. 56(3):251-2.
Kato I, Franco P, Grosswasser J, Scaillet S, et al. 2003. Incomplete arousal processes in infants who were victims of sudden death. Am J Respir Crit Care Med 168: 1298-1303.
Kennaway DJ, Goble FC and Stamp GE. 1996. Factors influencing the development of melatonin rhythmicity in humans. Journal of Clinical Endocrinology & Metabolism, Vol 81, 1525-1532
Korte J, Hoehn T, Siegmund R. 2004. Actigraphic recordings of activity-rest rhythms of neonates born by different delivery modes. Chronobiol Int. 21(1):95-106.
Logan RW and McClung CA. 2019. Rhythms of life: circadian disruption and brain disorders across the lifespan. Nat Rev Neurosci. 20(1):49-65.
Lohr B, Siegmund R. 1999. Ultradian and circadian rhythms of sleep-wake and food-intake behavior during early infancy. Chonobiology international 16(2): 129-148.
Matsuoka M, Segawa M, and Higurashi M. 1991. The Development of Sleep and Wakefulness Cycle in Early Infancy and Its Relationship to Feeding Habit. The Tohoku Journal of Experimental Medicine 165 (2):147-154.
McNamara F, Lijowska AS, and Thach BT. 2002. Spontaneous arousal activity in infants during NREM and REM sleep. J Physiol 538: 263-269.
Mirmiran M, Maas YG, Ariagno RL. 2003. Development of fetal and neonatal sleep and circadian rhythms. Sleep Med Rev. 7(4):321-34.
Nishihara K, Horiuchi S, Eto H, Uchida S. 2000. The development of infants’ circadian rest-activity rhythm and mothers’ rhythm. Psychiatry Clin Neurosci. 54(3):305-6.
Pecora G, Focaroli V, Paoletti M, Barca L, Chiarotti F, Borghi AM, Gasparini C, Caravale B, Bombaci I, Gastaldi S, Bellagamba F, Addessi E. 2022. Infant sleep and development: Concurrent and longitudinal relations during the first 8 months of life. Infant Behav Dev. 67:101719.
Pinilla T and Birch LL. 1993. Help me make it through the night: Behavioral entrainment of breasfed infants’ sleep patterns. Pediatrics 91: 436-444.
Poblano A, Haro R, and Arteaga C. 2007. Neurophysiologic measurement of continuity in the sleep of fetuses during the last week of pregnancy and in newborns. Int J Biol Sci. 4(1):23-8.
Quillin SI and Glenn LL. 2004. Interaction between feeding method and co-sleeping on maternal-newborn sleep. J Obstet gynecol Neonatal Nurs 33(5): 580-588.
Rivkees SA, Mayes L, Jacobs H, Gross I. 2004. Rest-activity patterns of premature infants are regulated by cycled lighting. Pediatrics. 113(4):833-9.
Sadeh A, Dark I, and Vohr BR. 1996. Newborns’ sleep-wake patterns: the role of maternal, delivery and infant factors. Early Hum Dev. 44(2):113-26
Sadeh A, Mindell JA, Luedtke K and Wiegand B. 2009. Sleep and sleep ecology in the first 3 years: a web‐based study. J Sleep Res 18: 60–73.
Siegel JM. 2005. Functional implications of sleep development. PLoS Biology 3(5): 756-758.
Srimoragot M, Hershberger PE, Park C, Hernandez TL, Izci Balserak B. 2022. Infant feeding type and maternal sleep during the postpartum period: a systematic review and meta-analysis. J Sleep Res. 2022 May 12:e13625.
Teng A, Bartle A, Sadeh A and Mindell J. 2012. Infant and toddler sleep in Australia and New Zealand. J. Paediatrics Child. Health 48: 268–273.
Thomas KA and Burr R. 2002. Preterm infant temperature circadian rhythm: possible effect of parental cosleeping. Biol Res Nurs. 3(3):150-9.
Torres-Farfan C, Rocco V, Monsó C, Valenzuela FJ, Campino C, Germain A, Torrealba F, Valenzuela GJ, and Seron-Ferre M. 2006. Maternal melatonin effects on clock gene expression in a nonhuman primate fetus. Endocrinology. 147(10):4618-26.
Touchette E, Dionne G, Forget-Dubois N, Petit D, Pérusse D, Falissard B, Tremblay RE, Boivin M, and Montplaisir JY. 2013. Genetic and environmental influences on daytime and nighttime sleep duration in early childhood. Pediatrics 131(6):e1874-80.
Tsai SY, Thomas KA, Lentz MJ, Barnard KE.2012. Light is beneficial for infant circadian entrainment: an actigraphic study. J Adv Nurs. 68(8):1738-47.
Tuladhar CT, Schwartz S, St John AM, Meyer JS, Tarullo AR. 2021. Infant diurnal cortisol predicts sleep. J Sleep Res. 30(6):e13357.
van Schaik SDM, Mavridis C, Harkness S, De Looze M, Blom MJM, and Super CM. 2020. Getting the Baby on a Schedule: Dutch and American Mothers’ Ethnotheories and the Establishment of Diurnal Rhythms in Early Infancy. New Dir Child Adolesc Dev. 2020(170):13-41.
Van Sleuwen BE, Englelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TWJ, and L’Hoir MP. 2007. Swaddling: A systematic review. Pediatrics 120: e1097-1106.
Wahnschaffe A, Haedel S, Rodenbeck A, Stoll C, Rudolph H, Kozakov R, Schoepp H, and Kunz D. 2013. Out of the lab and into the bathroom: evening short-term exposure to conventional light suppresses melatonin and increases alertness perception. Int J Mol Sci. 14(2):2573-89.
Wong SD, Wright KP Jr, Spencer RL, Vetter C, Hicks LM, Jenni OG, LeBourgeois MK. 2022. Development of the circadian system in early life: maternal and environmental factors. J Physiol Anthropol. 41(1):22.
Wulff K, Siegmund R. 2002.[Emergence of circadian rhythms in infants before and after birth: evidence for variations by parental influence]. Z Geburtshilfe Neonatol. 206(5):166-71. Review. German.
Zotter H, Urlesberger B, Pichler G, Mueller W, Kerbl R. 2007. Do wet diapers induce arousals in sleeping infants? Acta Paediatr. 96(3):452-3.
Content of “Newborn sleep patterns” last modified 1/5/23. Portions of this text derive from and earlier version of this article, written by the same author.
Image credits for “Newborn sleep patterns”
title image of father feeding newborn at night while mother sleeps by ArtMari / shutterstock
illustration of the SCN receiving input, image #6613, by the NIGMS, U.S. government, public domain
image of mother smiling while lying down with baby on a couch by Image Source / istock
image of father holding newborn by wong yu liang / shutterstock
image of newborn with outstretched arms by Ursula Page / shutterstock
image of mother breastfeeding by Tomsickova Tatyana / shutterstock
image of very tired new mother bottlefeeding her baby by Chanintorn.v / shutterstock















